HIV in Kenya: high risk groups aren't getting the attention they need
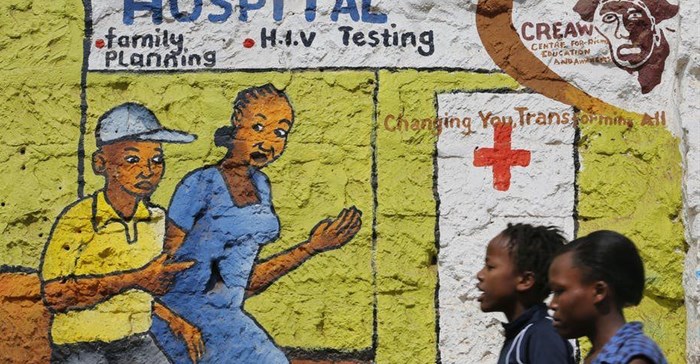
Kenya is one such country where the culture is conservative and homosexuality is generally a taboo subject. Gay people who are open about their sexuality are subjected to significant stigma and discrimination. This legal status, coupled with social stigma, makes it difficult for at-risk populations to seek preventive services in public health care facilities. In Kenya, key populations, including men who have sex with men and transgender women, contribute a third of new HIV infections.
In 2017, the Kenyan ministry of health launched a programme to provide pre-exposure prophylaxis (PrEP) to people at increased risk of HIV infection. PrEP is the use of anti-retroviral medication in HIV negative people as prevention against HIV. The aim of the programme is to make PrEP available at public health facilities. But this model may have shortcomings as men who have sex with men and transgender people may not feel comfortable in public health settings. Additionally, health care providers may not be prepared to provide services to key populations.
Healthcare providers refer to the national guidelines to determine who needs PrEP. But the guidelines don’t address anal sex. This is a major omission given that it carries the highest risk for HIV acquisition. And the guidelines assume that sexual behaviour is the same for all men who have sex with men. But, some may exclusively have sex with men, while others may also have sex with women. This difference in sexual behaviour has been shown to affect the risk of HIV acquisition.
We conducted a study to estimate HIV incidence among men who have sex with men exclusively, men who have sex with men and women as well as transgender women. We also wanted to assess how much interest there was in PrEP and what barriers there were to people accessing them.
Our research adds to existing knowledge about how behavioural differences can affect the risk of HIV acquisition. Our findings support the need to revise guidelines to better target PrEP at those that would most benefit for it.
The research
As part of the research we followed a cohort of men who have sex with men between 2016 and 2017 in Malindi on the coast of Kenya. We collected social demographic, sexual orientation and gender identity data that allowed us to classify participants as being either men who have sex with men and women or men who have sex with men exclusively or transgender women. We also explored participants’ knowledge and desire to take up PrEP.
Additionally, we assessed the factors associated with HIV acquisition. Finally, we held focus group discussions with HIV negative participants that were segregated by sexual orientation and gender identity.
Overall, the risk for HIV acquisition in this cohort over a one year period was 5%. But in transgender women this risk was extremely high at 20%. HIV acquisition was associated with a number of factors including exclusive receptive anal intercourse and history of a sexually transmitted infection.
A majority (98.8%) of the participants were interested in initiating PrEP. Transgender women expressed concern that actual PrEP provision may cause them to engage in condomless anal or group sex more frequently.
These results show a number of significant patterns. These include confirmation of a much higher risk of HIV acquisition in transgender women than in men who have sex with men.
Globally, studies have shown that transgender women have the highest risk of HIV acquisition. They also bear a disproportionate burden of HIV prevalence. The existence of transgender women has been generally ignored in most of sub-Saharan Africa. Transgender women are not a recognised key population in Kenya and may have previously been classified incorrectly as men who have sex with men exclusively.
Way forward
Our findings confirm that transgender women would benefit most from PrEP. But legal barriers and stigma mean that they are invisible and under-served in Kenya.
Read more:
Homosexuality remains illegal in Kenya as court rejects LGBT petition
We believe that our findings could be used to inform policy makers on the need to revise national guidelines to better target the intended recipients of the PrEP programme in Kenya. We hope to raise awareness on the need to recognise the existence of transgender women and the need for their inclusion in HIV prevention activities in Kenya.
This article is republished from The Conversation under a Creative Commons license. Read the original article.![]()
Source: The Conversation Africa

The Conversation Africa is an independent source of news and views from the academic and research community. Its aim is to promote better understanding of current affairs and complex issues, and allow for a better quality of public discourse and conversation.
Go to: https://theconversation.com/africa






















